theatlantic.com: Where the Opioids Go
10/24/2017
The rate of death from opioid overdoses in the United States has more than doubled over the past decade. Amid a deluge of reports on the national crisis, it’s easy to lose sight of the fact that in much of the world many people die in preventable pain, without access to morphine for end-of-life care.
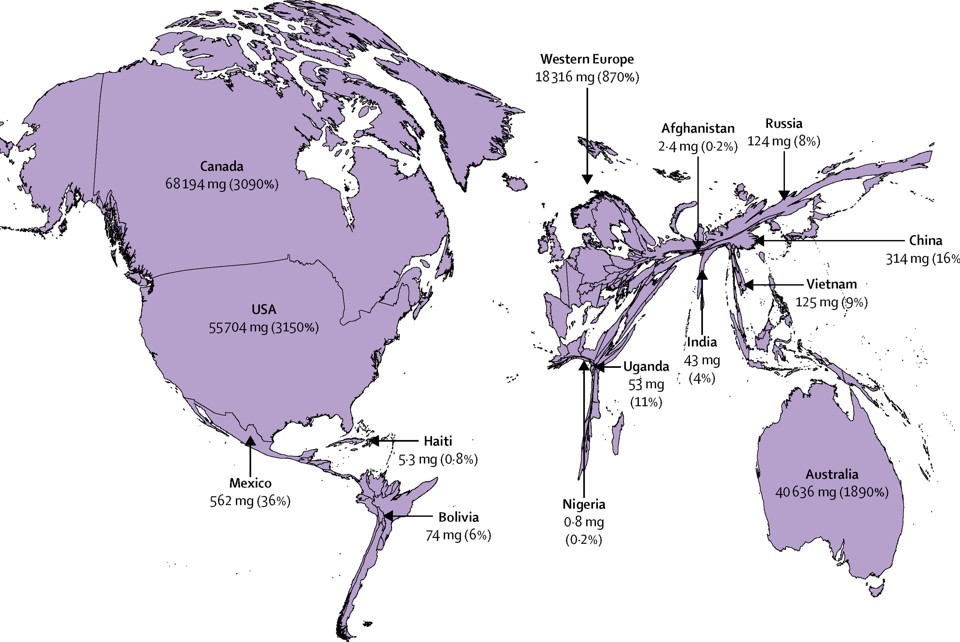
This is the finding of a global commission published in The Lancet, which includes analysis of the global distribution of narcotics. The above map shows a relative distribution of how much of the need for opioids is met in various places.
The focus of the report is addressing a relatively new target in global health, “serious health-related suffering” as a measure of the need for care. Palliative care, specifically, “should be focused on relieving the serious health-related suffering that is associated with life-limiting or life-threatening conditions or the end of life,” the authors write.
The idea is that suffering isn’t always preventable, but a few cents’ worth of morphine can make an enormous difference. Some 45 percent of the 56.2 million people who died in 2015 experienced serious suffering, the authors found. That included 2.5 million children. More than 80 percent of the people were from developing regions, and the vast majority had no access to palliative care and pain relief.
The authors conclude that the American opioid-overdose epidemic must be addressed in the same stroke as the narcotic famine: “A well-functioning and balanced global system must both prevent nonmedical use and misuse of medicines and ensure effective access to essential medicines for palliative care, including opioids for pain relief.”
That would involve including morphine in something called an Essential Package of palliative care and pain-relief interventions “to remedy the abyss in access to care.” These medications could be administered not just by doctors and nurses, but also by trained community health workers. The packages would be integrated into national health systems as part of universal health coverage, with the global scale helping make the model cost-effective.
They recommend immediate-release oral and injectable morphine for severe pain, which costs pennies per dose. At that rate, the “pain gap” could be closed for $145 million. This is less than some American pharmaceutical companies spend in any given year on marketing. To that end, the commission recommends prohibiting drug companies from marketing to patients or care providers—as the U.S. epidemic was driven by heavy marketing of powerful, expensive narcotics to address relatively moderate pain.
The United States stands as an outlier among wealthy countries in that it does not have a universal health-care system. As the country debates whether health care is a right, many objections come down to different understandings of what constitutes care—what it means to have a right to life and pursuit of happiness. The concept of serious health-related suffering may come to play in that discussion. Even the most austere fiscal conservatives have been reluctant to say that people with acute emergencies should be turned away from hospitals to die in the streets.
Access to morphine at the end of life would seem an area of agreement that transcends ideology—where the suffering of millions of people could be prevented at very little cost. Yet on a global scale, that’s not happening.